|
Supervised by: Prof Dino A. Giussani (dag26@cam.ac.uk) and Prof. Andrew J. Murray (ajm267@cam.ac.uk) |
|
|
Project Title: Placenta-related pregnancy complications and future female heart disease risk |
|
| Host Department: Department of Physiology, Development and Neuroscience (PDN) | |
|
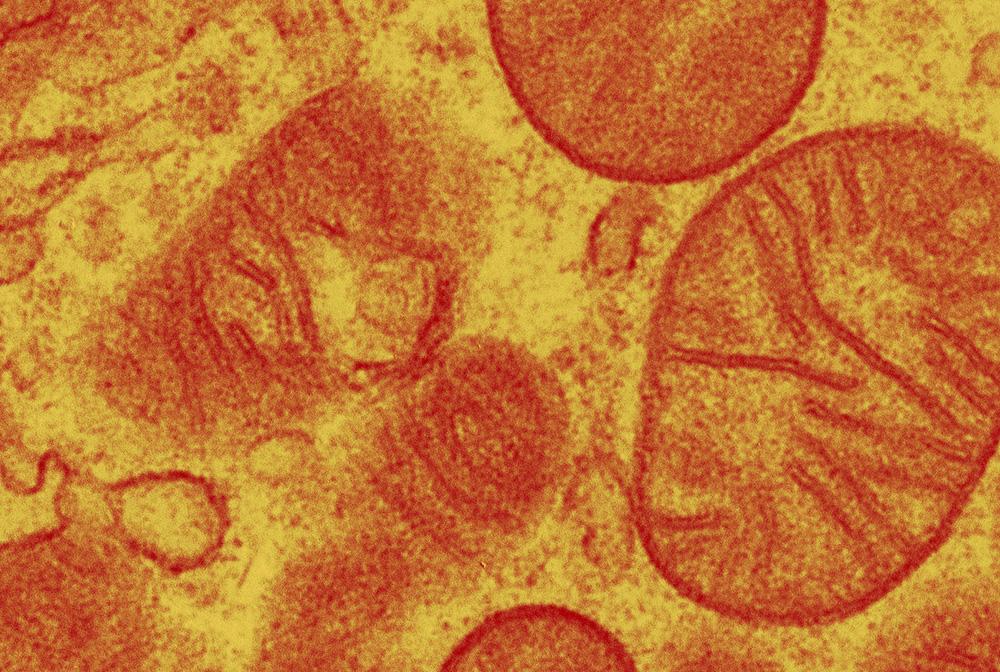
Project description Despite heart disease being one of the leading killers of women in the world, women continue to be underdiagnosed, undertreated, and underrepresented in cardiovascular science, with research failing to sufficiently address factors that uniquely affect a woman’s risk. This is particularly evident in young women and underserved populations such as lower socioeconomic and ethnic minority groups (1). One sex-specific condition that increases cardiovascular risk in women is pregnancy. It is well established that women who develop a complicated pregnancy, such as preeclampsia and/or fetal growth restriction, are at greater risk of cardiometabolic dysfunction during pregnancy and more susceptible to heart disease long after birth (2). However, it is unclear whether this is due to some women having a genetic predisposition to cardiometabolic dysfunction that is brought to the surface by pregnancy, or something about the complicated pregnancy that alters the susceptibility of genetically non-predisposed women to cardiac pathology. Our published work has reported that hypoxic pregnancy in sheep without prior cardiovascular risk mimics the utero-placental pathology associated with obstetric syndromes, such as preeclampsia and fetal growth restriction (3). However, whether these ewes develop cardiovascular complications during pregnancy and long after birth remains unknown. In particular, how altered mitochondrial substrate utilisation and respiratory capacity contribute to (patho)physiological changes in cardiac structure and function is completely unknown. This is critical, as there is an established link between cardiac bioenergetics and function, which ultimately determines disease risk and outcome. New unpublished work using echocardiography techniques shows that ewes exposed to hypoxic pregnancy relative to controls show cardiac dysfunction and structural remodelling not only during pregnancy, but also 6 months after giving birth. These unpublished work supports that mothers from complicated pregnancy are at greater risk of cardiovascular disease because of placentally-related complications of pregnancy rather than from genetic predisposition. This PhD Studentship will link cardiac mitochondrial bioenergetic mechanisms to the cardiac functional and geometric data at term and 6 months after birth in different cohorts of sheep which have experienced control or hypoxic pregnancy. Mitochondrial respiratory function, including substrate metabolism and electron-transport-chain function, will be studied in myocardium using novel protocols developed and optimised by our groups (4,5). Substrate/uncoupler/inhibitor titrations will be used to probe respiratory function using the Oroboros Oxygraph-2K. Electron flux through complex I will be supported by NADH, before succinate is added to additionally support flux through complex II. Rotenone is added to inhibit complex I and restrict electron flux to complex II. Complex IV-supported respiration will then be assessed, with O2 consumption expressed relative to both tissue mass and citrate synthase activity, to indicate respiratory capacity per mitochondrial unit. Spectrophotometric assays will be used to probe glycolysis, lactate production and fatty acid oxidation capacities, whilst gene/protein expression will be used to further probe mechanisms. The work will lead to a better understanding of the relationship between cardiac mitochondrial bioenergetics and echocardiographic indices of cardiac dysfunction. This will provide an opportunity for early cardiovascular risk stratification and the introduction of prophylactic strategies to better serve women experiencing adverse pregnancy. |
|
|
References
|
|

