|
Supervised by: Catherine Aiken (cema2@cam.ac.uk) & Sue Ozanne (seo10@cam.ac.uk) |
|
|
Project Title |
Impact of metformin use in early pregnancy on the placenta |
|
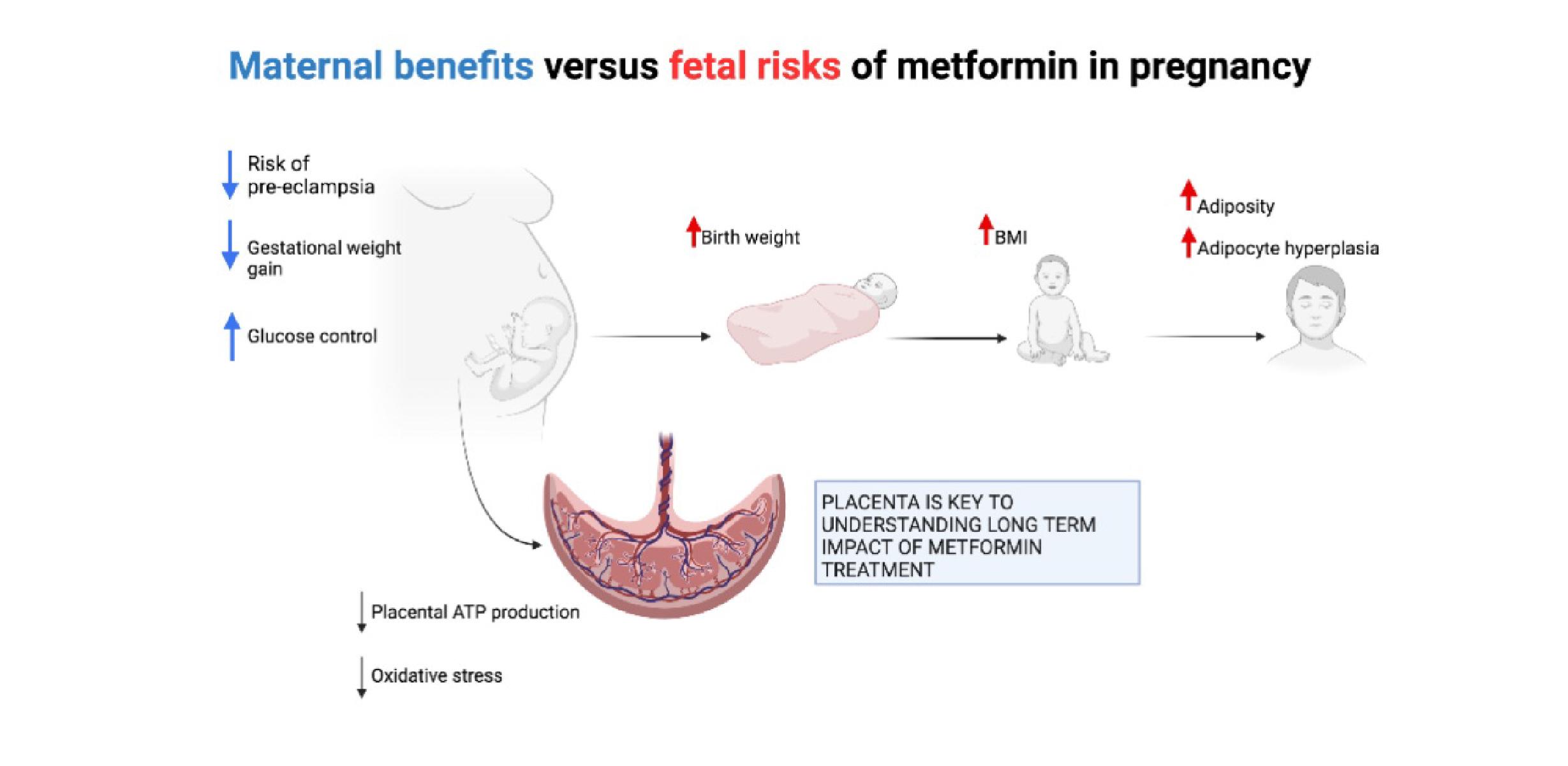
Project description Metformin is one of the most commonly prescribed drugs during pregnancy worldwide. It is primarily used in late pregnancy to treat gestational diabetes, but in recent years a growing number of women have been exposed to metformin during early pregnancy, particularly in the context of pre-pregnancy type 2 diabetes and during fertility treatment. There has also been growing international interest in metformin as a potential treatment or preventative drug for pre-eclampsia, which would be started early in pregnancy. We have previously shown 1 that pregnancies randomised to metformin treatment are less likely to develop pre-eclampsia, and other promising evidence suggests that metformin may improve outcomes in cases of severe pre-eclampsia 2. However the mechanism underlying these effects remains uncertain and there is very little understanding of how metformin exposure during early pregnancy might impact on placental function and metabolism. In our mouse model of metformin exposure during later pregnancy, fetal growth restriction is observed 3, in tandem with structural placental changes 3. It is currently unknown whether similar or more profound changes may occur when metformin treatment is started during early pregnancy. In late pregnancy, metformin significantly alters placental metabolic function in a negative manner, in particular reducing electron transport chain activity and ATP generation 4. However in early pregnancy, the placenta tends to rely more heavily on nonoxidative metabolism, potentially due to high sensitivity to reactive oxygen species 5. In this very different metabolic milieu, it is not clear how metformin might impact on the multiple biosynthetic and signalling functions that the placenta performs during the first trimester to ensure successful pregnancy and if effects impact positively or negatively on the feto-placental unit. During this project, the student will explore the metabolic and synthetic capabilities of first trimester trophoblast in response to metformin treatment. They will use both established mouse models and human-derived organoids to investigate a series of linked research questions: The project will give the student the opportunity to develop skills in working with both human organoid culture and rodent models of human disease. Support will be given to learn a wide range of molecular biology techniques, in addition to other key transferable skills including data analysis and scientific writing. The over-arching aim of the project will be to shed light on how metformin impacts placental function and development in the first trimester. This will fill an essential knowledge gap regarding whether metformin might plausibly be investigated as a preventative treatment for pre-eclampsia, a major cause of maternal and fetal mortality globally. It will also provide important new information on the potential impacts of using metformin in early pregnancy for other reasons, where the risk versus benefit ratio of doing so may be less clear-cut. |
|
|
References
|
|

